Intercept 3 – Jails and Courts
Proper training to improve outcomes for individuals with mental health and substance use challenges is especially important for those incarcerated and/or navigating the court system.
Intercept 3 – Jails and Courts
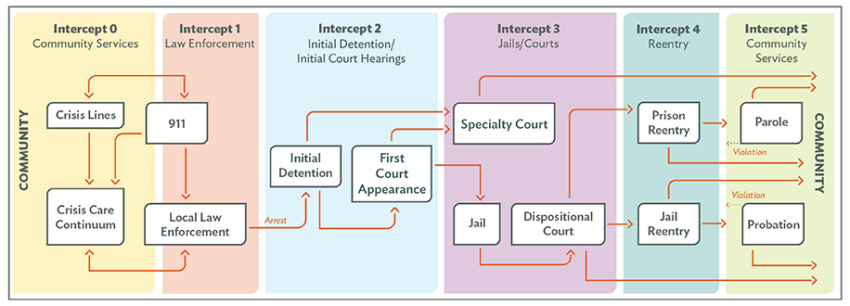
If an individual was not diverted at intercept 1 or 2, they progress to Intercept 3: Jails and Courts. This intercept includes detention at pretrial, during trial, prison after trial and sentencing as applicable. It is crucial that intercept 3 staff become competent in multiple core competencies to prevent the worsening of mental health and substance use challenges while in detention or incarcerated, as these events serve as major disruptions to individuals’ routines and can be traumatic in themselves. These transitions also put individuals more at risk of traumatic experiences while in jail or prison.
It is further recommended that staff become familiar with the Assess, Plan, Identify and Coordinate (APIC) model as part of the competencies for this intercept as well, as this has been proven to help coordinate reentry services. Jails and prisons are often in need of additional funding, training and clinical services to help prevent the onset/worsening of mental health/SUD symptomatology.
Intercept 3 CCBHC Integration Opportunities
- Court diversion programs for persons with MH/SU needs, including but not limited to specialty courts
- Jail-based programming and health care services
- Collaboration with specialist from the Veterans Health Administration
CCBHCs are required to establish care coordination partnerships with juvenile and criminal justice agencies and facilities (including drug, mental health, veterans and other specialty courts). While 33% of CCBHCs deliver direct services in courts, police offices and other justice-related facilities, 98% of CCBHCs accept referrals from courts, with 76% actively participating in specialty courts. And although Medicaid funding cannot be used to deliver direct services in jails, many CCBHCs are providing jail-based services through grants or other sources of funding. CCBHCs are also required to partner with local Veterans’ Affairs facilities to support military members, as their care is a component of CCBHCs’ required scope of service.
Intercept 3 Core Competencies
Collaboration and Teamwork
- Adopt a single system-wide county definition of key terms consistently used by local behavioral health systems, jails, courts and community corrections, including but not limited to:
- Substance use disorders
- Serious mental illness
- Recidivism
- Conduct a Sequential Intercept Model mapping workshop.
- Identify service capacity/interventions/gaps.
- Understand respective roles and responsibilities.
- Obtain leadership commitment (criminal justice council or task force).
- Develop collaborative criminal justice and behavioral task force if one does not already exist.
Workforce Development
- Improve correctional health care services for people who are incarcerated.
- Evidence-based SUD treatment, including agonist-based medication for opioid use disorder
- Trauma Informed Care (TIC)
- Cognitive Behavioral Therapy (CBT)
- Motivational Interviewing
- Family support
- Peer Navigators/Recovery Coaches
- Vocational training
- Educational services
- Identify evidence-based interventions and best practices for improving the health of people who are incarcerated:
- Medication Assisted Treatment (Long Acting Injectables)
- Medications for Opioid Use Disorder (MOUD)
- TIC
- Motivational Interviewing
- CBT
- Housing services
- Family support
- Vocational training
- Literacy training
- Education and employment assistance/support
- Peer Navigators/Recovery Coaches
- Naloxone distribution at release
- Linkage to community-based health care services
- In-reach services to connect people to health insurance and other services
- Provide cross-systems training on:
- Substance Use Disorder and Medication Assisted Treatment (MAT
- Implicit bias
- Data and evaluation
- Trauma-informed Care
- MHFA for public safety
- Motivational Interviewing
- SBIRT
- Peer Navigators/Recovery Coaches
- Integrated mental health treatment for co-occurring substance use disorders
- Administering naloxone to reverse opioid overdose
Screening and Assessment
- Assess the individual’s health and social needs and public safety risk.
- Implement validated screening and assessment tools and an efficient screening and assessment process.
- Inclusive of social determinants screenings and assessments
- Recommendation to utilize the Risk, Needs, Responsivity (RNR) Model and ensure alignment with behavioral health treatment approach.
- Criminogenic risk
- Substance use/misuse
- Mental illness
- Share assessment information with partners to streamline workflow and coordinate care.
- Utilize the Assess, Plan, Identify and Coordinate (APIC) Model to coordinate reentry services.
- Develop process for linking to services (warm handoffs).
- Plan for the treatment and services required to address the individual’s needs, both in custody and upon reentry.
- Inclusive of in-reach services related to Medicaid suspension/enrollment and other care coordination.
Care Planning and Care Coordination
- Utilize the Assess, Plan, Identify and Coordinate (APIC) Model to coordinate reentry services.
- Develop process for linking to services (warm handoffs).
- Plan for the treatment and services required to address the individual’s needs, both in custody and upon reentry.
- Inclusive of in-reach services related to Medicaid suspension/enrollment and other care coordination.
Cultural Humility
- Apply and address across remaining categories once competent in these principles:
- Implement/enhance anti-racist training and education.
- Adapt services to language, gender and pronoun preferences and cultural norms of population served.
- Develop task force that is inclusive of individuals with lived experience to spearhead the implementation/assessment of anti-racist policies and procedures, training and education.
Racial and Ethnic Disparities
- Identify and address racial disparities within criminal justice system involvement and in health care access and quality for populations served.
- Develop task force for racial and ethnic disparities to help achieve the following goals:
- Set qualitative process and outcome goals for racial and ethnic disparity reduction.
- Set a numerical target for reducing justice system involvement and/or improving outcomes for Black, Indigenous and people of color (BIPOC).
- Set a numerical target for reducing the relative likelihood of justice system involvement for BIPOC compared to White adults.
Evaluation and Quality Improvement
- Develop a city/county-level training plan that includes quality assurance to ensure fidelity.
- Develop a city/county-level plan for information/data sharing.
- Data Collection Across the Sequential Intercept Model (SIM): Essential Measures
- Agree on how to measure recidivism and other health outcomes. For example:
- Recidivism outcomes:
- Reduction in police contact, arrest and reincarceration.
- Health outcomes:
- Reduction in wait time for accessing services.
- Track no-shows.
- Track medication refills.
- Rate of homelessness upon release/access to housing.
- Reduction in hospitalization/ER rates.
- Increase access to care coordination.
- Reduction in wait time for Medicaid reinstatement.
- Recidivism outcomes:
Funding and Sustainability
- Prioritize policy, practice and funding improvements.
- Understand Medicaid/SSA coverage.
- Routinely communicate with the people responsible for the county budget.
- Utilize data to justify funding.
- Explore federal funding opportunities.
National Council Resources
- 2021 CCBHC and Justice Systems Report
- 2022 CCBHC Impact Report
- Addressing Health Equity and Racial Justice Resource Directory
- Health Equity Resource Directory
- Trauma-informed, Recovery-oriented Systems of Care Toolkit
- The Intersection of Criminal Justice, Race and Addiction: The Case of Harold Easter
- Medication-Assisted Treatment (MAT) for Opioid Use Disorder in Jails and Prisons: A Planning and Implementation Toolkit
- Trauma-informed Care Screening and Assessment Toolkit
- Implementing Medication for Opioid Use Disorder in Jails and Prisons: Lessons from the Field
- Addiction Services in Corrections in a COVID-19 World
Want to Learn More?
- Substance Abuse and Mental Health Services Administration (SAMHSA): Assess, Plan, Identify, Coordinate (APIC) Implementation Guide
- SAMHSA: Principles of Community-based Behavioral Health Services for Justice-involved Individuals: A Research-based Guide
- Bureau of Justice Assistance’s Comprehensive Opioid, Stimulant and Substance Abuse Program: Peer Recovery Support Services in Correctional Settings
- National Center for State Courts (NCSC): Certified Community Behavioral Health Clinics (CCBHCs) and the State Courts
- Federal Probation Journal: Peer Recovery Support Services in New York Opioid Intervention Courts: Essential Elements and Processes for Effective Integration
- Justice Center: Advancing the Work of Peer Support Specialists in Behavioral Health-Criminal Justice Programming
Relias Online Courses
Click here to access a wide variety of on-demand courses to enhance your care.
