Burned-out mental health treatment and substance use care professionals call on lawmakers to act
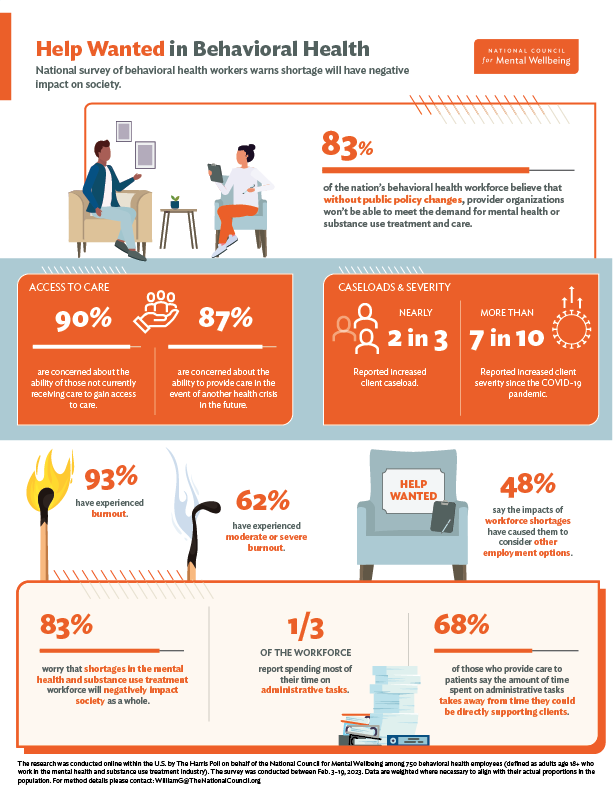
WASHINGTON, DC (April 25, 2023) — New survey data from the National Council for Mental Wellbeing, conducted by The Harris Poll, finds that the vast majority (83%) of the nation’s behavioral health workforce believes that without public policy changes, provider organizations won’t be able to meet the demand for mental health or substance use treatment and care. The survey, conducted among 750 behavioral health workers and more than 2,000 U.S. adults, also warns of a potential exodus of behavioral health workers due to burnout.
“As we prepare to observe Mental Health Awareness Month, we urge policymakers to listen to the voices of those in the field,” National Council for Mental Wellbeing President and CEO Chuck Ingoglia said. “Behavioral health organizations are seeing an increase in the severity of cases, and a backlog of young people in need of care has led to more youth being seen in emergency departments. Taking steps now to bolster the workforce through increased recruitment and retention efforts and the continued expansion of Certified Community Behavioral Health Clinics will give organizations that provide mental health treatment and substance use care the resources they need to meet capacity.”
KEY FINDINGS
- The vast majority (83%) of the nation’s behavioral health workforce believes that without public policy changes, provider organizations won’t be able to meet the demand for mental health or substance use treatment and care.
- Around nine in 10 behavioral health workers are concerned about the ability for those not currently receiving care to gain access to care (90%) and the ability to provide care in the event of another health crisis in the future (87%).
- Nearly two in three (65%) reported increased client caseload, and more than seven in 10 (72%) reported increased client severity since the COVID-19 pandemic.
- More than nine in 10 behavioral health workers (93%) said they have experienced burnout, and a majority report suffering from moderate or severe levels of burnout (62%).
- Nearly half (48%) of behavioral health workers say the impacts of workforce shortages have caused them to consider other employment options.
- More than four in five behavioral health workers (83%) worry that workforce shortages in the mental health and substance use industry will negatively impact society as a whole.
- A third of the workforce reported spending most of their time on administrative tasks, with 68% of those who provide care to patients saying the amount of time spent on administrative tasks takes away from time they could be directly supporting clients.
The National Council has identified numerous solutions to address workforce shortages in the field of mental health and substance use treatment and care, including:
1. Create a Behavioral Health Workforce Demonstration
Creation of a Behavioral Health Workforce Demonstration to help recruit and retain mental health and substance use treatment staff at critical safety net provider organizations. Given the high turnover and burnout rates, funding options to support retention bonuses, hazard pay, overtime and more could significantly support the retention and wellbeing of behavioral health workers.
2. Increase funding and expand national loan repayment programs
Increased funding for and expansion of national loan repayment programs, including the National Health Service Corps (NHSC), the NHSC Substance Use Disorder Workforce Loan Repayment Program (LRP) and the Substance Use Disorder Treatment and Recovery (STAR) LRP, to include those who provide care outside clinic walls and increased access to tuition assistance for the mental health and substance use fields similar to the Nurse Corps Scholarship Program. Currently, no such equivalent exists for the behavioral health workforce.
3. Further support the implementation and financing of CCBHCs
With the help of this innovation, clinics that became CCBHCs hired an average of 27 new positions per clinic and experienced an average 16% increase in their workforce.
4. Support Mental Health Access Improvement Act implementation
Support implementation of the Mental Health Access Improvement Act, legislation that was supported by the National Council and passed into law in late 2022. This legislation would allow marriage and family therapists and licensed professional counselors to bill Medicare and provide support for this sector of the workforce as they prepare for new billing structures and more.
5. Work to reduce unnecessary administrative burdens
Work with the administration to reduce unnecessary administrative burdens that contribute to burnout. The research found a third of the workforce reported spending most of their time on administrative tasks, with 68% of those who provide care to patients saying the amount of time spent on administrative tasks takes away from time they could be directly supporting clients.
DETAILED FINDINGS
Despite challenges created by the workforce shortage, a majority of those in the behavioral health field remain passionate about and fulfilled by their work. Nearly all employees are satisfied with their ability to make a difference for their clients (96%) and to help others at their current job (95%). However, workers say they face significant new challenges:
- Four in five (82%) say their passion for working in the industry is unwavering.
- Administrative tasks take away from time they could be directly supporting clients (68% of those who see clients and have administrative tasks).
- Their waitlist is longer than ever (58% of those who provide care to clients).
- They are seeing more than their ideal number of clients on a weekly basis (31% of those who provide care to clients).
- More than nine in 10 behavioral health workers (93%) said they have experienced burnout, and a majority report suffering from moderate or severe levels of burnout (62% reporting their level of burnout is an 8, 9 or 10 on a scale from 1 to 10 where 1 is no burnout at all and 10 is significantly burned out).
- Their work has had some negative impact on their life (80%), including their own mental health (37%).
- The impacts of workforce shortages have caused them to consider other employment options (48%).
The shortage shows no sign of easing. By 2025, the U.S. will be short about 31,000 full-time equivalent mental health practitioners, according to the Substance Abuse and Mental Health Services Administration (SAMHSA).

Behavioral health workers and the general public worry that the workforce shortage will negatively impact society. This comes at a time when access to care remains challenging and the number and severity of mental health and substance use cases has increased, due in part to the COVID-19 pandemic. The nation’s behavioral health workforce says a shortage of workers in the substance use and mental health field harms their ability to provide care and has made it more difficult for people to receive treatment, and large majorities of behavioral health workers and the general public worry about the impact of the workforce shortage on the health of the public:
- COVID-19 has led to increases in client severity (72%) and caseload (65%) among those who provide care to clients.
- More than four in five behavioral health workers (83%) and three-quarters of the general public (75%) worry that workforce shortages in mental health and substance use treatment will negatively impact society as a whole.
- More than eight in 10 behavioral health workers (84%) and nearly eight in 10 of the general public (78%) said people most in need of care have the most difficulty receiving it.
- Three-quarters of behavioral health workers (76%) fear the number of lives that will be lost due to lack of access caused by workforce shortages.
- Six in 10 (60%) say they are kept up at night thinking about those not able to access the care they need.
- Majorities of behavioral health workers are concerned about the ability for those not currently receiving care to gain access to the treatment they need (90%) or the ability to provide care in the event of another health crisis in the future (87%).
Behavioral health workers also said the following would help reduce the challenges in the mental health and substance use field created by the workforce shortages:
46%
more telehealth options
42%
apprenticeship programs
37%
student loan forgiveness
Additionally, 38% say less time spent on administrative tasks would help them better serve their clients.
“The workforce shortage is our top challenge and our top priority. It’s vital for the future of substance use care and mental health treatment that we have multiple avenues to attract and retain workers,” said Reyna Taylor, senior vice president of public policy and advocacy at the National Council for Mental Wellbeing. “So, we will continue to speak with lawmakers on both sides of the aisle and promote programs that improve recruitment and retention and promote self-care among the current work force.”
Methodology
The research was conducted online within the U.S. by The Harris Poll on behalf of the National Council for Mental Wellbeing among 750 behavioral health workers (defined as adults age 18+ who work in the mental health and substance use disorder treatment industry). The survey was conducted between February 3-19, 2023. Data are weighted where necessary to bring them in line with their actual proportions in the population. For method details please contact WilliamG@thenationalcouncil.org. The research also included a sample of the general public, to serve as a point of comparison. That research was conducted online February 7-9, 2023, among 2,080 adults ages 18+.
Download the Results
Enter your contact info to download a free copy of the Workforce Survey results. The PDF will open automatically when you click “submit.”
"*" indicates required fields
About The National Council
Founded in 1969, the National Council for Mental Wellbeing is a membership organization that drives policy and social change on behalf of over 3,100 mental health and substance use treatment organizations and the more than 10 million children, adults and families they serve. We advocate for policies to ensure access to high-quality services. We build the capacity of mental health and substance use treatment organizations. And we promote greater understanding of mental wellbeing as a core component of comprehensive health and health care. Through our Mental Health First Aid (MHFA) program, we have trained more than 4 million people in the U.S. to identify, understand and respond to signs and symptoms of mental health and substance use challenges.
Media Contact
Sophia Majlessi
Media@TheNationalCouncil.org
202-621-1631