Fostering Resilience and Recovery: Change Concept 4
Identify and Respond to Trauma Among Patients
Identifying and responding to different types of trauma requires a thoughtful approach tailored to the different experiences and needs of individual patients. Establishing patient trust and safety are critical to support disclosure and acceptance of trauma-related resources. Efforts to create safe environments, as described in Change Concept 1: Help All Individuals Feel Safety, Security and Trust, will facilitate more therapeutic and satisfying patient-provider relationships, which, in themselves, can be healing.
While disclosures of life-threatening situations require immediate response, disclosures of past trauma do not typically require an immediate intervention beyond a statement of empathy and an offer to talk more over time about its impact and available resources to address it. The process of trauma education, inquiry and response can help patients and providers better understand how trauma can lead to maladaptive coping behaviors, like substance misuse or overeating, and how those behaviors may negatively impact health and wellness.67 Ultimately, this understanding can lead to more satisfying and effective experiences of care for both patients and providers
Change Concept 4 Goals
- Patients have the opportunity to disclose and discuss the presence of significant past and current traumatic life events.
- Patients have opportunities to further assess (explore and discuss) in greater detail the impact of traumatic life events on their overall health and well-being.
- Our primary care service team offers patients trauma-related services in a timely manner, when needed.
- Our primary care service team collaborates with treatment provider to coordinate services for patients, when needed.
- Processes related to identifying and responding to trauma are culturally and linguistically appropriate.
- Our primary care service team develops service plans that build on patient strengths and address physical and emotional wellness.
Prepare for trauma inquiry and response
There are several steps to prepare to conduct trauma inquiry and response. These include:
- Establish policies and clinical pathways for identifying and responding to trauma.
- Develop an adequate referral network.
- Provide education to patients about the connection between trauma and health.
- Build staff capacity to conduct trauma inquiry and response.
- Prevent retraumatization among patients.
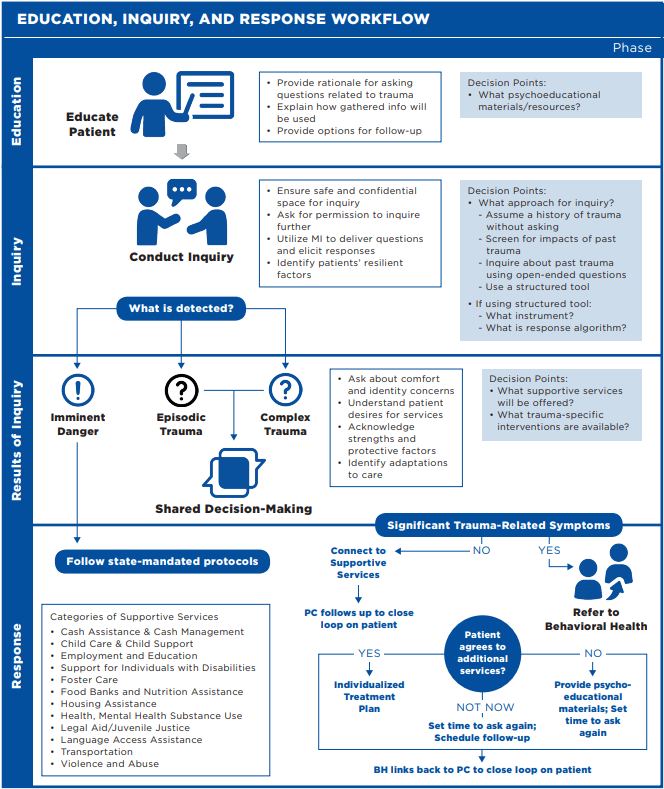
Many primary care providers transitioning to a trauma-informed approach have concerns about providing an adequate response when patients disclose experiences of trauma. It is common to hesitate to conduct inquiries about trauma as providers often do not feel that they have the tools and resources necessary to help individuals in need. Engaging in a conversation with a patient about trauma is similar to the way primary care providers approach other types of conditions. It is helpful to understand that while there are different types of trauma that necessitate different types of responses from providers, you can adequately serve most patients through a longer-term engagement with primary care and other health care professionals. Figure 1. illustrates an example education, inquiry, and response pathway; the full chapter provides comprehensive resources to operationalize these steps.
Inquire for and respond to recent trauma requiring immediate intervention
Your patients immediate safety is the top priority. It is essential that practices are prepared to address specific experiences of trauma including current abuse or violence, intimate partner violence (IPV), suicidal ideation and homicidal ideation. These situations require immediate assistance and compliance with mandated reporting laws (where applicable). An appropriate response when a patient discloses such an experience is to affirm that they do not deserve that treatment, express concern for the patient’s safety, explain that there are many helpful resources and follow mandated protocols while the patient is still onsite. You may offer a warm handoff to behavioral health staff or to a local agency providing specific services for their immediate needs.
Conduct inquiry for trauma
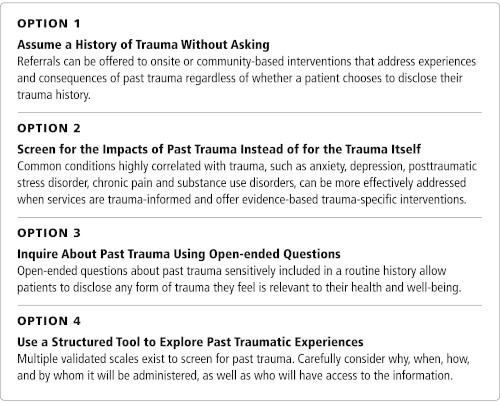
After preparing the clinical pathway and training staff, integrate inquiry for trauma into all appointments. Determine which approach best fits the needs of your patient population and is most appropriate for your level of integration. The figure below outlines four approaches to Trauma Inquiry, download the full chapter for more details.
When conducting inquiry with patients it is important to not only ask about challenges that might be affecting their lives, but also about the positive supports they have or the ways they have successfully coped in the past. In addition to inquiring about trauma, it is important for providers to identify patients’ positive strengths and resilient factors. Similar to inquiring about trauma, providers can use conversational and open-ended questions in addition to formalized instruments to inquire about resiliency.
It is helpful to understand that different types of trauma require different responses from providers. Patients who have experienced interpersonal, intimate partner or domestic violence; show signs of suicidal ideation; or are otherwise at risk of harm to themselves or others require an immediate response from providers. However, most patients who present with a history of trauma will not need immediate assistance and are adequately served with a longer-term engagement with primary care and other professionals. Table 10 provides recommended responses to different types of trauma.
| Type of Trauma | Examples | Response |
|---|---|---|
| Experiences of Trauma Requiring Immediate Intervention | Interpersonal violence, intimate partner violence or domestic violence. |
|
| Suicidal and homicidal ideation. | ||
| Experiences of Trauma | Episodic trauma: Exposure to an episodic or singular event that impacts an individual (e.g., car accident, robbery). More likely to lead to PTSD. |
|
| Complex trauma: Repetitive, prolonged or cumulative. Most often interpersonal, involving direct harm, exploitation and maltreatment. | ||
| Systemic trauma: Results from the contextual features of environments and institutions. |
Respond to trauma disclosures
Disclosures of trauma do not typically require detailed discussion or urgent intervention. Rather, responses to such disclosures are often best limited to a statement of empathy, an offer of available referrals to overcome the impacts of trauma and an opportunity to follow-up with you.
Adequate response to trauma disclosure includes a conversation with each patient about adaptations to care. By making small adjustments, you show respect for a patient that honors their concerns and prioritizes their voice in the treatment plan. In the following script, the provider creates an open space for the patient to share what they need to feel comfortable throughout the appointment. Examples of simple adaptations a patient may request include no fragrances in the exam room, a nurse present during sensitive exams and a phone call to discuss exam results rather than written results. If the patient does not have any specific requests at the time, emphasize that they can revisit this at future appointments. Note any identified adaptations in their health record and respect them at each appointment.
“In light of what you’ve shared today, is there anything I can do to make you feel more comfortable during our appointments together? Do you have any concerns we should address before moving forward? I will note it in the record for future appointments and you can always change or add to it later.”
Every patient’s treatment plan should utilize their strengths. Engaging in a process to identify strengths and incorporating them in their health care plan is a resilience-building strategy. Developing a plan together that is unique to their needs, goals and strengths increases self-confidence, hopefulness and participation in the treatment plan. Ask your patient about the people, places and activities they rely on to support their health and wellness. Identify their health strengths, including an awareness about preventive screenings, current health status, and strategies to manage personal stressors.
There are many evidence-based techniques and mental health interventions to help patients heal from the impacts of trauma and cope more healthfully and safely with ongoing symptoms and persistent traumas such as racism or xenophobia. Medical providers are not typically resourced or trained to lead these interventions; however, they have a crucial role in linking patients to treatments in the community or to onsite psychosocial staff members who are skilled in providing them.
Learning more about trauma-specific interventions can help providers identify what may be most useful to their patient. Trauma-specific interventions include individual and/or group therapies that help patients manage trauma symptoms, process traumatic experiences and/or reduce isolation; trauma-informed somatic interventions like yoga, mindfulness-based stress reduction, acupuncture and somatic experiencing therapy; and medicines and techniques, such as eye movement desensitization and reprocessing (EMDR), to reduce post-traumatic symptoms like insomnia, nightmares, anxiety and depression. Often, a combination of such interventions that lead to genuine healing.
It is important to note that many patients may not be interested in or able to tolerate trauma-specific interventions that require processing past traumatic events. Refer these individuals to the many trauma-specific services that do not involve directly processing trauma (e.g., drop-in support groups, dialectical behavioral therapy [DBT] and various forms of expressive and art-based therapies) that can start the healing process by helping patients connect with others and develop healthier coping skills. You can also support patients who do not want any trauma-related referrals to begin healing through faith and spirituality, exercise, nature, work, caring for people and pets and other practices that foster connection, comfort and meaning.


